It’s about a 5 min. read.
Now that the vaccine is available to every American, I’ve been thinking a lot about the activities I can’t wait to get back to, while also re-evaluating what I’m comfortable with. What have I truly missed doing and what are the new habits I’ve formed that may carry over into my “next normal”? For example, ordering groceries online to avoid shopping in-store is a new habit I plan on sticking with. Telehealth is another service that I, and many of us, are considering keeping in our routine for the long-haul. The technology has been around for nearly two decades, and yet, many like myself never used it until the pandemic.
We’ve certainly seen benefits to telehealth: less commuting, less wait time, and (from the patient side) more efficient service. The ability for providers to care for patients virtually has freed up space and helped to prioritize resources to treat patients with the most serious conditions for which in-person care is necessary. Thus, it’s no surprise that, according to McKinsey, providers are seeing 50 to 175 times the number of patients via virtual care solutions than they did before COVID-19, and the number of US consumers using telehealth grew from 11% in 2019 to 46% in 2020. Now that adoption and usage of virtual care has become more prevalent, will healthcare consumers continue this behavior in the “next normal”? According to that same study, 76% of consumers indicated that they are interested in using telehealth going forward.
Of course, there are services that can’t be handled virtually, but have behaviors changed so much that consumers are willing to forgo certain procedures? While most elective procedures were forced to be postponed in the early days of the pandemic outbreak, data has shown that visits for preventative screenings like colonoscopies and mammograms have also declined, which could lead to serious illnesses going undetected. In order for healthcare providers to best serve patients going forward, they need to understand the new habits formed during the pandemic that are going to stick and why, which segments are most likely to maintain new habits, and where can they influence good habits such that consumers are still getting the care they need.
That is why with CMB’s Habit Loops®, we measure people’s deeply ingrained routines—the driving motives, cues/triggers that inspire action, the experience of the behavior/routine itself, and the experiential/material or psychological rewards that ultimately lead to practicing that routine again.
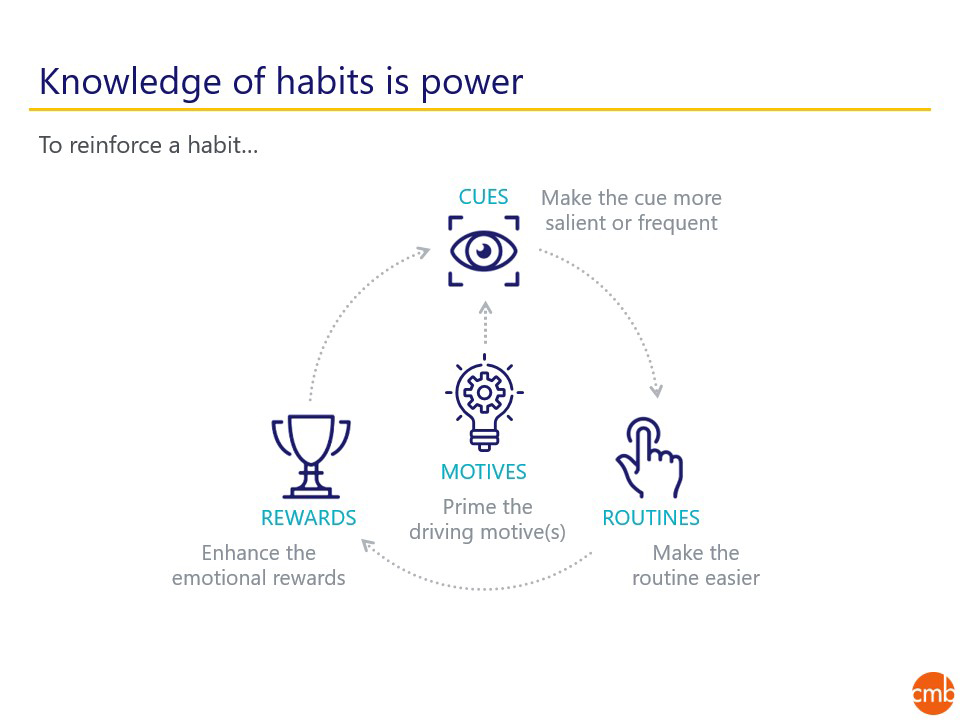
If there are certain virtual behaviors/routines that providers want to reinforce—to align with capacity, to see a return on their investment in upgraded technology, bandwidth or staff training, etc.—it will be important for them to make the routine of the telehealth visit easy and seamless so that it is worthwhile to the consumer such that they continue to use virtual services.
In practice, consider the scenario where a patient has a sore throat that they want to get checked out but are worried about being around other sick patients.
In the case of patients who have forgone specific procedures like preventative screenings because of pandemic-related concerns/barriers, measuring the habit loop is critical for providers to be able to re-engage these patients. You should ask yourself:
As we turn a corner with the vaccine roll out, plan for a digital-first world to stay. Providers should examine their messaging/marketing on their websites/digital portals to not only make sure it’s helping consumers navigate the tactical elements of their virtual care experience, but also considering the emotional elements to help patients feel empowered in their decision-making and feel secure/content in their decision to seek care virtually or in-person.
Healthcare providers have the power to influence or trigger habits that can be mutually beneficial to the provider and patient or disrupt habits that aren’t. By identifying the habits or elements of the routine that make a behavior easier or more rewarding, providers can better contribute to improving the patient experience, and achieve the ultimate goal of better patient outcomes/health.